Sensory processing characteristics of adults who have complex regional pain syndrome
I. Literature Review
Introduction
The purpose of this project was to explore complex regional pain syndrome (CRPS) by using current models of sensory modulation disorder (SMD) and by using narrative interview. Sensory processing theory as grounded in sensory integration theory (Ayres, 1979, p. 5) and later modified by Dunn (1997) provided the background neurophysiological models for this study. Dunn stated that there is a relationship between neurological sensory thresholds and observed behavior (1997). The Sensory Profile was used to provide an assessment of this relationship based on the report of patients who have CRPS. This type of test that measures behavioral responses was used in this study to inform a narrative inquiry to understand the impact that these disorders have on occupation.
Current scholars are integrating sensory integration theory into occupation-based intervention approaches by re-examining ways to broaden Ayres’ original concepts (Parham & Mailloux, 2001, p. 330). Although Ayres may not have explicitly described the impact that disordered sensory systems have on occupations, these concepts can be applied to develop a richer understanding of what it means to have sensory processing difficulties.
Some practice models identify the relationship between the individual, the occupation that is being performed, and the environment. The P-E-O model (Law, Cooper, Strong, Stewart, Rigby, & Letts, 1996) states that behavior can’t be separated from its contextual influences. This type of model was helpful in describing the relationships between personal/constitutional factors, chosen occupations, and illness factors for people who had CRPS.
My initial interest in this topic was generated by seeing patients who developed CRPS and learning that the recommended occupational therapy treatment protocols for this condition include sympathetic stress loading (Carlson & Watson, 1988; Phillips, Katz, & Harden, 2000). These protocols for sympathetic stress loading seemed very similar to the recently popularized “sensory diet” protocol (Wilbarger & Wilbarger, 2002, p. 335-338) used for people who had SMD. My familiarity with both patient populations of adult orthopedics and pediatrics provided perspective and interest in the topic. I continued to read extensively on the topic of pain and pain sensation, initially motivated after reading the groundbreaking work of Melzack & Wall (1965). My interest in the subject has never diminished and this has led me to the literature contained herein and the interest in completing this project.
Studies of sympathetically mediated pain provide evidence that hypotheses regarding central processing may be useful in describing the pathological mechanisms involved in CRPS. Still, a larger question that remains unanswered is whether or not there was an increased risk of developing CRPS because of the sympathetic processing differences or if those differences became evident as a function of the CRPS. To date, there have not been any predictive epidemiological studies of CRPS that would address this basic question.
There is potential utility for exploring the relationships between CRPS and sensory processing. First, if there is a population of people who have SMD and are more at risk for developing CRPS it could be helpful to know who they are so that early intervention could be attempted as soon as they incur an injury to a limb. Second, if there is an underlying mechanism of sensory processing dysfunction that predisposes people to CRPS, this would provide a more solid physiological explanation for what occupational therapists currently identify as SMD. The research that has been completed on CRPS may provide important information for helping occupational therapists understand SMD.
Although any implied linkages between these conditions are theoretical at this time, identifying common features of the disorders could assist in understanding them both at a deeper level.
Complex regional pain syndrome
Complex regional pain syndrome (CRPS) is a disorder characterized by chronic pain that is disproportionate to the trauma that caused the pain. It is important for clinicians to be able to understand different types of pain, and there are clear distinctions between acute nociceptive pain and chronic pain. Nociceptive pain is related to the degree of receptor stimulation that is caused by a specific tissue injury, and involves the normal activation of the nociceptive system by noxious stimuli (Kandel & Jessell, 1991, p. 386-7). By contrast, chronic pain may occur by continued irritation of the nociceptors, which can cause neuroactive, biochemical, inflammatory, or vasoactive effects such as histamine release that can activate or increase the sensitivity in the cellular/receptor environment (p. 386). Over time, peripheral to central processing may also modify nociception, (p. 389-92) and behavioral/emotional states may also influence the perception of pain (p. 398). Chronic pain syndromes can often lead to long-term disability and loss of occupational functioning; for this reason they have been studied extensively and are of interest to occupational therapy practitioners.
Classification
Complex regional pain syndrome has been called many different names such as reflex sympathetic dystrophy, causalgia, and Sudeck's atrophy. This disorder commonly occurs in the limbs following an injury. Typical features include dramatic changes in the color and temperature of the skin over the affected limb or body part, intense burning pain, skin sensitivity, sweating, swelling, decreased joint mobility, and changes in nail and hair growth patterns (NINDS, 2003).
The International Association for the Study of Pain developed a classification system that delineates CRPS into two distinct categories (Stanton-Hicks, Janig, Hassenbusch, Haddox, Boas, & Wilson, 1995). In CRPS I the individual may experience regional pain and sensory changes following a trauma. In CRPS II there is also regional pain and sensory changes but a nerve lesion is identifiable. CRPS I is classically associated with the previous entity defined as reflex sympathetic dystrophy; CRPS II is associated with the previously defined condition of causalgia (Baron & Wasner, 2001).
Etiology
There has been considerable debate regarding the etiology and pathophysiology of CRPS. Sympathetically maintained and sympathetically independent pain categories are phenomena that are referenced in the current classification system (Stanton-Hicks, Janig, Hassenbusch, Haddox, Boas, & Wilson, 1995). Sympathetically mediated pain is typically identified by its amelioration after treatment of sympathetic-blocking intervention, while sympathetically independent pain does not (Manning, 2000). However, it is unclear if these two classes are entirely independent of each other or if they can occur at the same time. This distinction may be important in understanding and developing intervention for CRPS.
Several researchers have investigated sympathetic nervous system functioning in patients who have complex regional pain syndromes. Specifically, several studies indicate that the nervous systems of people who have these syndromes are measurably different than normal. For example, normal inhibitory influences on pain during sympathetic arousal are compromised in the majority of patients with CRPS (Drummond, Finch, Skipworth, & Blockey, 2001). Evidence also exists that patients who have sympathetically mediated chronic pain have widely spread prefrontal hyperactivity, increased activity in the anterior cingulate, and decreased contralateral thalamic activity as measured by functional magnetic resonance imaging (Apkarian, Thomas, Krauss, & Szeverenyi (2001).
Another hypothesis is that there is brain reorganization in the primary somatosensory cortex of patients who have CRPS and that the degree of neural reorganization as measured by magnetoencephalography is directly related to the degree of pain (Maihofner, Handwerker, Neundorfer, & Birklein, 2003). Another study identified a change in the central representation of somatosensation, most likely in the thalamus or cortex, and that sensory threshold are higher on the affected side of the body in people who have CRPS (Rommel, Malin, Zenz, & Jänig (2001).
Preliminary studies demonstrate that brain imaging scans are different for people who have CRPS (Juottonen, Gockel, Silen, Hurri, Hari, & Forss, 2002). Other authors (Schwoebel, Friedman, Duda, & Coslett, 2001) found functional neurological changes in patients who have CRPS. Specifically, they state that patients who have CRPS have impaired body schema involving their painful limbs, suggest atypical processing of proprioceptive, somatosensory, and vestibular sensory inputs. These studies provide evidence that hypotheses regarding central processing may be useful in describing the pathological process involved in CRPS.
Differences in neuroendocrine functioning may explain some alterations in central processing of somatosensory inputs. Janig & Baron (2002) state that nociceptor hyperexcitability may be facilitated by sympathetically-released norepinepherine, which in turn may generate a state of central excitability that causes spontaneous and secondary evoked pain. Therefore, the pain and sensory changes seen in CRPS I may be the result of distorted processing of information in the central nervous system involving the somatosensory pathways.
The pattern of progression of symptoms has also been useful in generating hypotheses about the mechanisms underlying these disorders. For example, Maleki, LeBel, Bennett, and Schwartzmann (2000) describe patterns including contiguous spread, independent spread, and mirror spread. Contiguous spread represents localized progression of symptoms close to the initial injury site. Independent spread represents general nervous system susceptibility for CRPS evidenced by symptoms in distal/unrelated parts of the body. Mirror spread represents contralateral processing errors where symptoms are noted on the opposite side of the body to where the injury occurred. These differing patterns all represent different neurological processing of responses to the initial injury.
Some research is beginning to investigate genetic predisposition for developing CRPS. Janig & Baron (2003) and Wasner, Schattschneider, Binder, & Baron (2003) both reviewed studies that identified possible genetic causes. The studies that have been completed are preliminary; controversy remains regarding the role of genetic factors on this disease.
The presence of psychological factors in people who have CRPS has led to ongoing speculation that there may be a psychological basis for these disorders. A biopsychosocial model (Van Houdenhove & Vasquez, 1993) of CRPS suggests that loss of occupational functioning can lead to helplessness, which in turn causes passive coping and stress-related sympathetic overreactivity and higher norepinephrine levels. The authors suggest that these factors contribute to worsening of symptoms. However, although stress responses may exacerbate symptoms it is now generally accepted that there is no common psychological profile of people who have CRPS (Lynch, 1992). Rather, it is believed that CRPS leads to anxiety and depression rather than anxiety and depression leading to CRPS. This is a phenomenon that continues to be the subject of interesting research that has mixed results. For example, Harden et.al. (2003) found that preoperative distress and pain had modest utility in predicting CRPS signs, although there was a high rate of false positive identification. More research is needed to help clarify the relationship between psychological profile, psychogenic predisposition, and CRPS.
Diagnostic tests for CRPS
Diagnostic testing that identifies common parameters of physiologic functioning could be helpful in investigating the possible intersection of CRPS and SMD. However, there is no specific diagnostic test for CRPS. Several medical tests can be used to assist in the diagnosis. Bone scans (Schiepers, 1997) use radiation to identify areas of bone where there may be abnormalities. Infrared thermography (Gulevich, et.al., 1997) measures relative temperature distributions in the limb which may provide information about blood flow and sympathetic activity. Axon reflex testing (Chelimsky, et.al., 1995; Low, Caskey, Tuck, Fealey, & Dyck, 1983), and resting skin temperature/resting sweat output (Chelimsky, et.al., 1995) have also been described in the literature. These are nervous system tests that provide specific information regarding autonomic functioning. Selective tissue conductance (National Pain Foundation, 2003) is a newer diagnostic test that measures galvanic skin responses but it has not been well researched.
In some cases, a sympathetic nerve block can be used to diagnose CRPS in patients with clinical evidence of sympathetically mediated pain; however, not all CRPS is due to sympathetic nerve dysfunction (Rho, Brewer, & Wilson, 2002). Some researchers have tried to identify patients who are at higher risk for CRPS based on other factors including psychological profile, genetics, and sensory processing but none of these are widely accepted and used for diagnostic purposes.
Diagnosis is generally made by the presence of clinical signs and symptoms including dramatic changes in the color and temperature of the skin over the affected limb or body part, intense burning pain, skin sensitivity, sweating, swelling, decreased joint mobility, and changes in nail and hair growth patterns (NINDS, 2003). Additionally, the physician will gather important patient history and rule out any other conditions.
Diagnostic tests for sensory modulation disorders
Pfeiffer & Kinnealey (2003) describe the use of the Adult Sensory Questionnaire (Kinnealey & Oliver, 2002) to determine degree of sensory modulation difficulty but this tool is not widely accessible or commonly used. Kinnealey & Fuiek (1999) also used the Adult Sensory Questionnaire and proposed a model of interrelationship between SMD, anxiety, depression, and pain perception in adults although they noted that more research was needed to clarify these relationships. Preliminary studies (McIntosh, Miller, Shyu, & Hagerman, 1999) support the presence of a physiological basis of SMD, finding that electrodermal responses were larger in children with SMD, excepting those who were non-responders. Additionally, children with atypical electrodermal responses had more parent-reported abnormal behavioral responses to sensation. Miller, et.al. (1999) identified Fragile X syndrome as a clinical condition where baseline hyperarousal may exist because unimodal over-reaction predicted hyperarousal in other sensory modalities. Additionally, Schaaf, Miller, Sewell, & O'Keefe (2003) found that cardiac vagal tone index was significantly decreased for children who had identified sensory processing difficulties. These studies provide preliminary evidence that there is a physiological basis for SMD. All of these studies used the Sensory Challenge Protocol (Miller, et.al., 1999) which is a research tool and is not designed for clinical application. A single case study (Reisman & Gross, 1992) using physiological markers of an adult has also been reported to identify improvements following intervention for SMD.
The Sensory Profile is a standardized assessment used by occupational therapists “to measure a child’s sensory processing abilities and to profile the effect of sensory processing on functional performance in the daily life of a child” (Dunn, 1999, p. 1). Dunn states that there is a relationship between neurological sensory thresholds and observed behavior (1997). The Sensory Profile (Dunn, 1999) provides an assessment of this relationship based on the report of the child’s parent. The Adolescent/Adult Sensory Profile (Brown & Dunn, 2002) provides an assessment of this relationship based on self-report. These measures are the most widely used and widely accepted standards used by occupational therapists for assessing SMD.
Summary of diagnostic tests
Both CRPS and SMD are disorders that are not easily identified and are typically diagnosed through the use of tools that involve clinical observations of presenting symptoms or a report of those symptoms. Researchers often measure neurophysiologic characteristics to determine the presence of each disorder. Many of those neurophysiologic markers are common to both disorders in that they represent altered sympathetic/autonomic functioning; however, most of those tests are not easy to administer in a clinical environment.
The Adolescent/Adult Sensory Profile (AASP) represents a behavioral self-report of sensory processing. The AASP measures four quadrants of sensory processing as identified by Brown and Dunn (2002). The four quadrants include sensation seeking, sensation avoiding, sensory sensitivity and low registration. Preliminary studies suggest that this format of assessment is an accurate predictor of altered neurophysiologic functioning. Specifically, this four quadrant model was validated through expert rating and skin conductance testing (Brown, Tolefson, Cromwell, & Filion, 2001).
The AASP is easy to administer and it is non-invasive. As there seem to be common underlying features of CRPS and SMD relating to altered sympathetic functioning, this assessment may be clinically useful for predicting sympathetic hyperarousal that may potentially lead to CRPS. Additionally, if the assessment is sensitive enough to identify the relationship between CRPS and SMD it may provide evidence of a common underlying neurological deficit between the two conditions.
Face validity for the use of the AASP for predicting CRPS
The Adolescent/Adult Sensory Profile is a sixty item self report questionnaire designed as a “trait measure” (Brown & Dunn, 2002, p.1) of sensory processing, meaning that the individual is supposed to answer regarding how they generally respond to sensory stimulation. It does not measure specific response patterns to specific sensory stimulation. The AASP measures responsivity across categories of taste/smell processing, movement processing, visual processing, touch processing, activity level, and auditory processing (p.2). From these scores the assessment provides a profile of sensory processing across four quadrants: low registration, sensation seeking, sensory sensitivity, and sensation avoiding (p.1.). Dunn’s Model of Sensory Processing (1997) is used to explain the relationship between altered neurological thresholds and the impact that this has on daily life functioning.
Based on previously identified evidence of altered sensory thresholds leading to pain and hyperarousal in people who have CRPS, it seems reasonable to apply Dunn’s model to this population. Although the exaggerated state of sympathetic arousal in people who have CRPS is not clinically identical to hyperarousal in people who have SMD, these two conditions may constitute a continuum of pathology that is reflective of sympathetic nervous system dysfunction.
Literature review does not provide information regarding any possible connections between these disorders, although the presence of parallel studies that examine neurophysiologic/sympathetic markers is intriguing. Occupational therapists who understand these two conditions may assist in elucidating common features that will assist in understanding both CRPS and SMD. The significance of this inquiry is considerable. The ability to identify the population of people who are ‘at-risk’ for developing CRPS would be invaluable for clinical purposes of intervention planning. The significance of this is even greater if this can be determined through the use of a non-invasive self-report questionnaire like the AASP. Additionally, there is only beginning physiologic rationale and understanding of SMD. If a link is present between these disorders CRPS may provide an interesting presentation of sensory-affective hyperarousal that can help occupational therapists better understand SMD and how it impacts occupation.
Summary
Complex regional pain syndrome and sensory modulation disorder are clinically distinct entities that are often treated by different populations of occupational therapists. As a result, there has not been any literature describing or exploring any intersection of these disorders. There has not been any documentation of discussion regarding the intervention strategies that overlap and address similar underlying components of both disorders.
Both disorders are poorly understood, but hyperarousal and excessive sympathetic nervous system outflow are suspected as being significant contributors to both of these disorders. Sympathetic stress loading techniques are commonly used as intervention for both conditions.
Occupational therapy researchers are conducting studies regarding neurophysiologic parameters that would help to quantify sympathetic nervous system hyperarousal. Similar testing techniques have already been used in researching complex regional pain disorders.
Because of multiple points of commonality, assessment strategies useful for sensory modulation disorders may provide useful clinical information regarding complex regional pain syndrome. In turn, these points of commonality could provide a stronger basis of neurophysiologic rationale behind the explanation of sensory modulation disorders.
This paper describes an initial attempt at investigating the intersection of these two disorders. Researching the similarities between these two conditions provides useful clinical information that can lead to better understanding of the disorders and improved intervention strategies and patient outcomes.
II. Methodology
Sample size and composition:
Five subjects were identified for participation in the study. The subjects were all over eighteen years of age. Subject criteria stated that they could be either male or female, but had to be English speaking and residents of the Counties of Erie or Niagara in New York State. All subjects had to have a current diagnosis or recent history of complex regional pain syndrome secondary to orthopedic injuries including fractures, ligament or tendon injuries, or peripheral nerve damage.
The principal investigator provided eligibility criteria to the lead therapist at the ABC Therapeutics facility in Lockport, NY. Based on the criteria, the lead therapist used purposive sampling to develop a subject eligibility list. Subjects were then given an invitation to participate in the study. After subjects expressed interest to participate in the study, all personal and confidential information was de-identified and presented to the principal investigator. Patient charts were never viewed by the principal investigator.
Purposive sampling was used with specific selection criteria as follows: all subjects had to have current or historical clinical signs of complex regional pain syndrome; they had to be over 18 years of age at the time of their initial injury, and they were drawn from the patient pool at a private occupational therapy practice in Lockport, New York. None of the subjects will be patients of the principal investigator. Maximum variation sampling was used regarding subject gender, underlying orthopedic condition, educational attainment, and job title.
Informed consent:
Subjects who expressed an interest in participating were contacted for an appointment to discuss the study with the principal investigator and to sign the informed consent paperwork. During this appointment the principal investigator provided informed consent information to the subject to read. The principal investigator answered all questions relating to the study and the informed consent forms and followed the format as listed on the signature sheets. Once the informed consent process was completed, the subjects were invited to stay to complete the two assessments. Additional appointment times to accommodate the subject’s schedules were provided, as necessary.
Methods and Procedures
Following selection and informed consent processes, the principal investigator provided subjects with the Adolescent/Adult Sensory Profile (AASP) (Brown & Dunn, 2002) to complete. The AASP is a standardized assessment used by occupational therapists to measure sensory processing abilities and to profile the effect of sensory processing on functional performance in daily life. Dunn states that there is a relationship between neurological sensory thresholds and observed behavior (1997). The AASP (Brown & Dunn, 2002) provides an assessment of this relationship based on self-report. This measure is the most widely used and widely accepted standard used by occupational therapists for assessing SMD in adults.
Following completion of the AASP, the principal investigator administered the Canadian Occupational Performance Measure (COPM) to the subject. The COPM (Law, et. al., 1990) is an individualized, client-centered measure designed for use by occupational therapists. The COPM measures self-care, productivity and leisure outcomes. Clients rate themselves on performance and satisfaction with performance.
It is primarily designed to be used as a clinical outcome measure and is cited extensively in the occupational therapy literature. The COPM showed good evidence of concurrent criterion validity and sensitivity to change when used to measure performance after client participation in a pain management program (Carpenter, Baker, & Tyldesley, 2001).
The authors of the COPM identify that it can also be used as a measure of occupational performance in research (Law, et. al., 1990). Specifically, the authors suggest that the COPM is useful for studies aimed at understanding the determinants of occupational performance problems as well as for explanatory studies that try to show relationship between occupation and other variables. For purposes of this study, the COPM was administered once to obtain data on the subject’s perception regarding occupational performance difficulties. It was chosen for this study specifically because it elicited information regarding quality of life and satisfaction with current occupational participation (Liddle & McKenna, 2000).
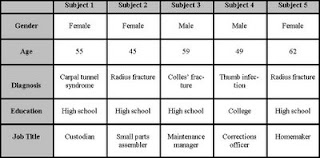
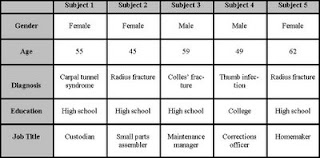
Although purposive and maximum variation sampling strategies were used, the subject pool had some common characteristics. In summary, they were all within the range of 45-65 years of age. All of the subjects had a diagnosis of complex regional pain syndrome secondary to an injury. Their job titles were significantly variable and although three of the five subjects had distal upper extremity fractures, not all of them were caused by work injuries. Only one subject had education beyond high school. Three women and two men agreed to participate in the study.
The following table outlines demographic characteristics of the subject pool.
Using descriptive methods, information obtained from the AASP was graphically tabulated and analyzed to report frequencies and distributions of scores. Information from the COPM was analyzed with identical methods to report frequencies and distributions of self-reported occupational performance difficulties. Information from the COPM provided additional narrative information that assisted in descriptive analysis.
III. Results
The subjects were given the Adolescent/Adult Sensory Profile to complete. The AASP classifies responses into categories of Low Registration, Sensation Seeking, Sensory Sensitivity, and Sensation Avoiding. Scores are classified as being much less than most people, less than most people, similar to most people, more than most people, and much more than most people.
Low registration refers to a pattern of sensory processing that is characterized by high sensory thresholds and a passive self regulation strategy (Dunn, 1997). Three of the five subjects scored differently than the normative group. Two had a greater degree of low registration and one had a lower degree of low registration.
Sensation seeking refers to a pattern of sensory processing that is characterized by high sensory thresholds and an active self regulation strategy (Dunn, 1997). Two of the five subjects had lower sensation seeking scores than the normative group.
Sensory sensitivity refers to a pattern of sensory processing that is characterized by low sensory thresholds and a passive self regulation strategy (Dunn, 1997). Two of the five subjects scored differently than the normative group: one had a greater degree of sensory sensitivity and one had a lower degree.
Sensation Avoiding refers to a pattern of sensory processing that is characterized by low sensory thresholds and an active self regulation strategy (Dunn, 1997). One subject scored lower than the normative group and one scored much lower than the normative group. Another subject scored much higher than the normative group.
The following table summarizes score performance of the subject pool.

Finally, the subjects were given the Canadian Occupational Performance Measure to complete. Using the COPM scoring card the client was asked to rate the importance of each chosen activity on a scale of 1-10, (1 as not important at all and 10 as extremely important). After reviewing the ratings with the client, the top five highest scored, self- perceived problems were scored for performance and satisfaction. These were also rated on a scale of 1-10. Each score was then divided by 5 (the number of problems identified by the client).
The following table summarizes reported scores of the subject pool.

As indicated in the chart below, the most common problems highlighted by the subjects were inability to complete various aspects of dressing occupations (8 prioritized problems) and inability to work at all (5 prioritized problems). In the leisure category, two subjects specifically identified inability to participate in grandparenting occupations as a prioritized problem. The remaining prioritized problems scattered around individual tasks within the three occupational domains.

IV. Discussion
In this small sample there was evidence that all of the subjects had areas of atypical sensory processing as measured by the AASP. However, there was absolutely no consistency whatsoever in the pattern and distribution of scores on this test. The AASP measures sensory processing differences in a bidirectional manner – meaning that scores can either be higher or lower than the normative range and are considered atypical in either direction away from the mean. However, the nature of that atypicality is dependent on the directionality of difference of the scores.
As identified in the literature review there is some evidence of altered sensory thresholds leading to pain and hyperarousal in people who have CRPS. However, there was not a significant pattern of sensory sensitivity that was seen in the AASP test scores of the subjects. There are several factors that could explain why this relationship was not observed.
First, there may in fact be no relationship to CRPS hyperarousal and pre-existing sensory sensitivity as measured by the AASP. The literature provides strong face validity to the hypothesis that sensory sensitivity and the associated active sensory avoiding behaviors might be associated with the sensory processing of people who have CRPS. However, the patients in this study may have been at different stages with their CRPS and in part that could account for differences in their AASP responses. Very acute CRPS could potentially bias sensory sensitivity responses, where chronic CRPS may not.
Additionally, although the tactile hypersensitivity factors account for a degree of overall hypersensitivity scores, there are other sensory channels that are considered on the AASP. So simple tactile hypersensitivity is only a component of overall sensory sensitivity and may not be enough to trigger identification as in the sensory sensitivity quadrant on the AASP.
Second, the sample size may be too small to identify a reliable measure of sensory processing tendencies of the group. So although it is interesting that the scores of the subjects all were atypical, it is not possible to draw conclusions on this finding at this time.
It may be possible that people who have CRPS are more likely to have sensory processing disturbances that manifest atypically in directions of both hyper and hypo-arousal and responsivity. The AASP measures both behavioral responses and actual sensory perceptions. Depending on an individual’s passive or active coping strategy the nature of the difficulty may be more complex than a simple univariate model that is explained by sensitivity associated with heightened avoidance strategies. Additional research is warranted to elucidate the scoring patterns observed in this initial probe.
More directly, the subject’s prioritization and ranking of perceived occupational performance problems was clear. The subjects report significant problems with loss of ability to participate in preferred occupations, with self care being the greatest area of concern. Work and leisure concerns were also reported, but not at the same frequency. Not all disability or disease processes have a direct relationship to decreases in functional performance. In this case, whether or not there is any underlying relationship between sensory processing factors between CRPS and SMD, it is very clear that people who have these diagnoses experience significant occupational dysfunction. Self care skills and performance in daily activities are domains of concern for occupational therapists. The low COPM scores in perceived performance and satisfaction validates that people who have CRPS with SMD are good candidates for occupational therapy evaluation and intervention.
V. Summary
Complex regional pain syndrome and sensory modulation disorder are clinically distinct entities that are often treated by different populations of occupational therapists. As a result, there has not been any literature describing or exploring any intersection of these disorders. There has not been any documentation of discussion regarding the intervention strategies that overlap and address similar underlying components of both disorders.
Both disorders are poorly understood, but the literature indicates that hyperarousal and excessive sympathetic nervous system outflow are suspected as being significant contributors to both conditions. Sympathetic stress loading techniques are commonly used as intervention for both conditions. Occupational therapy researchers are conducting studies regarding neurophysiologic parameters that would help to quantify sympathetic nervous system hyperarousal. Similar testing techniques have already been used in researching complex regional pain disorders.
Because of these multiple points of commonality between the conditions, assessment strategies useful for sensory modulation disorders were used in this study to obtain additional clinical information regarding complex regional pain syndrome. Although there was no single pattern of sensory processing disorder for people who had CRPS, it was clear that they all had some degree of atypical sensory processing as measured by the AASP. Additionally, all of the subjects who had CRPS had significant occupational dysfunction as measured on the COPM.
VI. Conclusion
The research that has been completed on CRPS provides useful information for occupational therapists to consider when investigating sensory modulation disorders. This literature review and exploratory study demonstrates that there is justification for continuing to study the possible relationship between disorders that share common sensory processing factors as they have a significant impact on people’s occupational function.
References:
Apkarian, A.V., Thomas, S., Krauss, B.R. and Szeverenyi, N.M. (2001). Prefrontal hyperactivity in sympathetically mediated chronic pain. Neuroscience Letters, 311, 193-197.
Ayres, A.J. (1979). Sensory integration and the child. Los Angeles: WPS.
Baron, R. & Wasner, G. (2001). Complex regional pain syndromes. Current Pain and Headache Reports, 5, 114-123.
Brown, C., Tolefson, N., W., Cromwell, R. & Filion, D. (2001). The adult sensory profile: Measuring patterns of sensory processing. American Journal of Occupational Therapy, 55, 75-82.
Brown, C.E. & Dunn, W. (2002). Adolescent/Adult Sensory Profile User’s Manual. San Antonio: The Psychological Corporation.
Carlson. L & Watson, H. K. (1988). Treatment of reflex sympathetic dystrophy using the stress loading program. Journal of Hand Therapy, 1, 149-154.
Carpenter, L. Baker, G.A. & Tyldesley, B. (2001). The use of the Canadian Occupational Performance Measure as an outcome of a pain management program. Canadian Journal of Occupational Therapy , 68(1), 16-22.
Chelimsky, T.C., Low, P.A., Naessens, J.M., Wilson, P.R., Amadio, P.C., O'Brien, P.C, (1995). Value of autonomic testing in reflex sympathetic dystrophy. Mayo Clinic Proceedings, 70, 1029-1040.
Drummond P.D., Finch, P.K., Skipworth, S., & Blockey, P. (2001). Pain increases during sympathetic arousal in patients with complex regional pain syndrome. Neurology 5, 1296-1303.
Dunn, W. (1997). The impact of sensory processing abilities on the daily lives of young children and their families: A conceptual model. Infants and Young Children, 9, 23-35.
Dunn, W. (1999). Sensory Profile User’s Manual. San Antonio: The Psychological Corporation.
Gulevich, S.J., Conwell, T.D., Lane, J., Lockwood, B., Schwettmann, R.S., Rosenberg, N., et.al. (1997). Stress infrared telethermography is useful in the diagnosis of complex regional pain syndrome, type I (formerly reflex sympathetic dystrophy), Clinical Journal of Pain, 13, 50-59.
Harden, R.N., Bruehl, S., Stanos, S., Brander, V., Chung, O.Y., Saltz, S. et.al. (2003). Prospective examination of pain-related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: A preliminary study. Pain, 106, 393-400.
Janig, W. & Baron, R (2002). Complex regional pain syndrome is a disease of the central nervous system. Clinical Autonomic Research, 12, 150-164.
Janig, W. & Baron, R (2003). Complex regional pain syndrome: mystery explained?
The Lancet Neurology, 2, 687-97.
Juottonen, K., Gockel, M., Silen, T., Hurri, H., Hari, R., & Forss, N. (2002). Altered central sensorimotor processing in patients with complex regional pain syndrome. Pain. 98, 315-23.
Kandel, E.R. & Jessell, T.M.(2001). Touch, in Kandel, E.R., Schwartz, J.H. & Jessell, T.M. (Eds.). Principles of Neural Science, 3rd ed. New York: Elsevier.
Kinnealey M.., Fuiek, M. (1999) The relationship between sensory defensiveness, anxiety, depression and perception of pain in adults. Occupational Therapy International. 6, 195-206.
Kinnealey, M. & Oliver, B. (2002). The Adult Sensory Questionnaire. Retrieved July 17, 2004 from http://www.temple.edu/OT/Neuro_Behavioral_Center2.htm
Law, M., Cooper, B., Strong, S., Stewart, D., Rigby, P., & Letts, L. (1996). The Person-Environment-Occupation Model: A transactive approach to occupational performance. Canadian Journal of Occupational Therapy, 63, 9-23.
Law, M., Baptiste, S., McColl, M.A., Opzoomer, A., Polatajko, H. & Pollock, N. (1990). The Canadian Occupational Performance Measure: An outcome measure for occupational therapy. Canadian Journal of Occupational Therapy, 57(2), 82-87.
Liddle, J & McKenna, K. (2000). Quality of Life: An overview of issues for use in occupational therapy outcome measurement. Australian Occupational Therapy Journal, 47, 77-85.
Low, P.A., Caskey, P.E., Tuck, R.R., Fealey, R.D., Dyck, P.J. (1983). Quantitative sudomotor axon reflex test in normal and neuropathic subjects. Annals of Neurology, 14, 573-580.
Lynch, M. (1992). Psychological aspects of reflex sympathetic dystrophy: a review of the adult and paediatric literature. Pain. 49, 337-347.
Maihofner C., Handwerker, H.O., Neundorfer, B., Birklein, F. (2003). Patterns of cortical reorganization in complex regional pain syndrome. Neurology, 61, 1707-15.
Maleki, J., LeBel, A.A., Bennett, G.J., & Schwartzman, R.J. (2000). Patterns of spread in complex regional pain syndrome, type I (reflex sympathetic dystrophy). Pain, 88, 259-66
McIntosh DN, Miller LJ, Shyu V, Hagerman RJ. (1999). Sensory-modulation disruption, electrodermal responses, and functional behaviors. Developmental Medicine and Child Neurology, 41, 608-15.
Melzack, R. & Wall, P. (1965). Pain mechanisms: A new theory, Science, 150, 171-179.
Miller L.J., McIntosh, D.N., McGrath, J., Shyu, V., Lampe, M., Taylor, A.K., et.al. (1999). Electrodermal responses to sensory stimuli in individuals with fragile X syndrome: A preliminary report. American Journal of Medical Genetics, 83, 268-79.
Miller, L. J., Reisman, J. E., McIntosh, D. N., & Simon, J. (2001). An ecological model of sensory modulation: Performance of children with fragile X syndrome, autistic disorder, attention-deficit/hyperactivity disorder, and sensory modulation dysfunction. In S. Smith-Roley, E. I. Blanche, & R. C. Schaaf (Eds.), Understanding the nature of sensory integration with diverse populations (pp. 57-88). San Antonio, TX: Therapy Skill Builders.
National Institute for Neurological Disorders and Stroke (2003). Complex Regional Pain Syndrome (also called Reflex Sympathetic Dystrophy Syndrome) Fact Sheet. Retrieved May 14, 2004 from http://www.ninds.nih.gov/health_and_medical/
pubs/rsds_fact_sheet.htm
National Pain Foundation (2003). How CRPS Happens. Retrieved June 3, 2004 from http://www.painconnection.org/cm/CMDisplayAllArticles.asp?ClassId=15&CategoryId=1
Parham, L.D. & Mailloux, Z. (2001). Sensory integration. In J.Case-Smith (Ed.), Occupational therapy for children (4th ed.). St. Louis: Mosby.
Pfeiffer, B. & Kinnealey, M. (2003) Treatment of sensory defensiveness in adults. Occupational Therapy International, 10, 175-184.
Phillips, M.E., Katz, J.A., & Harden, R.N. (2000). The use of nerve blocks in conjunction with occupational therapy for complex regional pain syndrome type I. American Journal of Occupational Therapy. 54, 544-549.
Reisman, J.E., & Gross, A.Y. (1992) Psychophysiological measurement of treatment effects in an adult with sensory defensiveness. Canadian Journal of Occupational Therapy, 59, 5248-5257.
Rho, R.H., Brewer, R.P., Lamer, T.J., Wilson, P.R. (2002). Complex regional pain syndrome. Mayo Clinic Proceedings, 77, 174-180.
Rommel, O., Malin, J., Zenz, M., & Jänig, W. (2001). Quantitative sensory testing, neurophysiological and psychological examination in patients with complex regional pain syndrome and hemisensory deficits. Pain, 93, 279-293.
Schaaf, R.C., Miller, L.J., Sewell, D., & O'Keefe, S. (2003). Children with disturbances in sensory processing: A pilot study examining the role of the parasympathetic nervous system. American Journal of Occupational Therapy, 57, 442-449.
Schiepers, C. (1997). Clinical value of dynamic bone and vascular scintigraphy in diagnosing reflex sympathetic dystrophy of the upper extremity. Hand Clinics, 13, 423-429.
Schwoebel, J., Friedman, R., Duda, N., Coslett, H.B. (2001). Pain and the body schema: evidence for peripheral effects on mental representations of movement. Brain, 124, 2098-104.
Stanton-Hicks, M., Janig, W., Hassenbusch, S., Haddox, J.D., Boas, R., Wilson, P. (1995). Reflex sympathetic dystrophy: Changing the concepts and taxonomy, Pain: 63, 127-133.
Van Houdenhove, B., & Vasquez, G. (1993). Is there a relationship between reflex sympathetic dystrophy and helplessness? General Hospital Psychiatry, 15, 325-329.
Wasner, G., Schattschneider, J., Binder, A., & Baron, R. (2003). Complex regional pain syndrome--diagnostic, mechanisms, CNS involvement and therapy. Spinal Cord. 41, 61-75.
Wilbarger, J.L. & Wilbarger, P.L. (2002). The Wilbarger approach to treating sensory defensiveness, In Bundy, A.C., Murray, E.A., & Lane, S. (Eds.). Sensory Integration: Theory and Practice, 2nd Ed., Philadelphia, PA.: F.A. Davis.
Acknowledgement
Many thanks to Dr. Carol Reed and Dr. Sandee Dunbar who both provided neverending encouragement, review, and editing for this project.
Introduction
The purpose of this project was to explore complex regional pain syndrome (CRPS) by using current models of sensory modulation disorder (SMD) and by using narrative interview. Sensory processing theory as grounded in sensory integration theory (Ayres, 1979, p. 5) and later modified by Dunn (1997) provided the background neurophysiological models for this study. Dunn stated that there is a relationship between neurological sensory thresholds and observed behavior (1997). The Sensory Profile was used to provide an assessment of this relationship based on the report of patients who have CRPS. This type of test that measures behavioral responses was used in this study to inform a narrative inquiry to understand the impact that these disorders have on occupation.
Current scholars are integrating sensory integration theory into occupation-based intervention approaches by re-examining ways to broaden Ayres’ original concepts (Parham & Mailloux, 2001, p. 330). Although Ayres may not have explicitly described the impact that disordered sensory systems have on occupations, these concepts can be applied to develop a richer understanding of what it means to have sensory processing difficulties.
Some practice models identify the relationship between the individual, the occupation that is being performed, and the environment. The P-E-O model (Law, Cooper, Strong, Stewart, Rigby, & Letts, 1996) states that behavior can’t be separated from its contextual influences. This type of model was helpful in describing the relationships between personal/constitutional factors, chosen occupations, and illness factors for people who had CRPS.
My initial interest in this topic was generated by seeing patients who developed CRPS and learning that the recommended occupational therapy treatment protocols for this condition include sympathetic stress loading (Carlson & Watson, 1988; Phillips, Katz, & Harden, 2000). These protocols for sympathetic stress loading seemed very similar to the recently popularized “sensory diet” protocol (Wilbarger & Wilbarger, 2002, p. 335-338) used for people who had SMD. My familiarity with both patient populations of adult orthopedics and pediatrics provided perspective and interest in the topic. I continued to read extensively on the topic of pain and pain sensation, initially motivated after reading the groundbreaking work of Melzack & Wall (1965). My interest in the subject has never diminished and this has led me to the literature contained herein and the interest in completing this project.
Studies of sympathetically mediated pain provide evidence that hypotheses regarding central processing may be useful in describing the pathological mechanisms involved in CRPS. Still, a larger question that remains unanswered is whether or not there was an increased risk of developing CRPS because of the sympathetic processing differences or if those differences became evident as a function of the CRPS. To date, there have not been any predictive epidemiological studies of CRPS that would address this basic question.
There is potential utility for exploring the relationships between CRPS and sensory processing. First, if there is a population of people who have SMD and are more at risk for developing CRPS it could be helpful to know who they are so that early intervention could be attempted as soon as they incur an injury to a limb. Second, if there is an underlying mechanism of sensory processing dysfunction that predisposes people to CRPS, this would provide a more solid physiological explanation for what occupational therapists currently identify as SMD. The research that has been completed on CRPS may provide important information for helping occupational therapists understand SMD.
Although any implied linkages between these conditions are theoretical at this time, identifying common features of the disorders could assist in understanding them both at a deeper level.
Complex regional pain syndrome
Complex regional pain syndrome (CRPS) is a disorder characterized by chronic pain that is disproportionate to the trauma that caused the pain. It is important for clinicians to be able to understand different types of pain, and there are clear distinctions between acute nociceptive pain and chronic pain. Nociceptive pain is related to the degree of receptor stimulation that is caused by a specific tissue injury, and involves the normal activation of the nociceptive system by noxious stimuli (Kandel & Jessell, 1991, p. 386-7). By contrast, chronic pain may occur by continued irritation of the nociceptors, which can cause neuroactive, biochemical, inflammatory, or vasoactive effects such as histamine release that can activate or increase the sensitivity in the cellular/receptor environment (p. 386). Over time, peripheral to central processing may also modify nociception, (p. 389-92) and behavioral/emotional states may also influence the perception of pain (p. 398). Chronic pain syndromes can often lead to long-term disability and loss of occupational functioning; for this reason they have been studied extensively and are of interest to occupational therapy practitioners.
Classification
Complex regional pain syndrome has been called many different names such as reflex sympathetic dystrophy, causalgia, and Sudeck's atrophy. This disorder commonly occurs in the limbs following an injury. Typical features include dramatic changes in the color and temperature of the skin over the affected limb or body part, intense burning pain, skin sensitivity, sweating, swelling, decreased joint mobility, and changes in nail and hair growth patterns (NINDS, 2003).
The International Association for the Study of Pain developed a classification system that delineates CRPS into two distinct categories (Stanton-Hicks, Janig, Hassenbusch, Haddox, Boas, & Wilson, 1995). In CRPS I the individual may experience regional pain and sensory changes following a trauma. In CRPS II there is also regional pain and sensory changes but a nerve lesion is identifiable. CRPS I is classically associated with the previous entity defined as reflex sympathetic dystrophy; CRPS II is associated with the previously defined condition of causalgia (Baron & Wasner, 2001).
Etiology
There has been considerable debate regarding the etiology and pathophysiology of CRPS. Sympathetically maintained and sympathetically independent pain categories are phenomena that are referenced in the current classification system (Stanton-Hicks, Janig, Hassenbusch, Haddox, Boas, & Wilson, 1995). Sympathetically mediated pain is typically identified by its amelioration after treatment of sympathetic-blocking intervention, while sympathetically independent pain does not (Manning, 2000). However, it is unclear if these two classes are entirely independent of each other or if they can occur at the same time. This distinction may be important in understanding and developing intervention for CRPS.
Several researchers have investigated sympathetic nervous system functioning in patients who have complex regional pain syndromes. Specifically, several studies indicate that the nervous systems of people who have these syndromes are measurably different than normal. For example, normal inhibitory influences on pain during sympathetic arousal are compromised in the majority of patients with CRPS (Drummond, Finch, Skipworth, & Blockey, 2001). Evidence also exists that patients who have sympathetically mediated chronic pain have widely spread prefrontal hyperactivity, increased activity in the anterior cingulate, and decreased contralateral thalamic activity as measured by functional magnetic resonance imaging (Apkarian, Thomas, Krauss, & Szeverenyi (2001).
Another hypothesis is that there is brain reorganization in the primary somatosensory cortex of patients who have CRPS and that the degree of neural reorganization as measured by magnetoencephalography is directly related to the degree of pain (Maihofner, Handwerker, Neundorfer, & Birklein, 2003). Another study identified a change in the central representation of somatosensation, most likely in the thalamus or cortex, and that sensory threshold are higher on the affected side of the body in people who have CRPS (Rommel, Malin, Zenz, & Jänig (2001).
Preliminary studies demonstrate that brain imaging scans are different for people who have CRPS (Juottonen, Gockel, Silen, Hurri, Hari, & Forss, 2002). Other authors (Schwoebel, Friedman, Duda, & Coslett, 2001) found functional neurological changes in patients who have CRPS. Specifically, they state that patients who have CRPS have impaired body schema involving their painful limbs, suggest atypical processing of proprioceptive, somatosensory, and vestibular sensory inputs. These studies provide evidence that hypotheses regarding central processing may be useful in describing the pathological process involved in CRPS.
Differences in neuroendocrine functioning may explain some alterations in central processing of somatosensory inputs. Janig & Baron (2002) state that nociceptor hyperexcitability may be facilitated by sympathetically-released norepinepherine, which in turn may generate a state of central excitability that causes spontaneous and secondary evoked pain. Therefore, the pain and sensory changes seen in CRPS I may be the result of distorted processing of information in the central nervous system involving the somatosensory pathways.
The pattern of progression of symptoms has also been useful in generating hypotheses about the mechanisms underlying these disorders. For example, Maleki, LeBel, Bennett, and Schwartzmann (2000) describe patterns including contiguous spread, independent spread, and mirror spread. Contiguous spread represents localized progression of symptoms close to the initial injury site. Independent spread represents general nervous system susceptibility for CRPS evidenced by symptoms in distal/unrelated parts of the body. Mirror spread represents contralateral processing errors where symptoms are noted on the opposite side of the body to where the injury occurred. These differing patterns all represent different neurological processing of responses to the initial injury.
Some research is beginning to investigate genetic predisposition for developing CRPS. Janig & Baron (2003) and Wasner, Schattschneider, Binder, & Baron (2003) both reviewed studies that identified possible genetic causes. The studies that have been completed are preliminary; controversy remains regarding the role of genetic factors on this disease.
The presence of psychological factors in people who have CRPS has led to ongoing speculation that there may be a psychological basis for these disorders. A biopsychosocial model (Van Houdenhove & Vasquez, 1993) of CRPS suggests that loss of occupational functioning can lead to helplessness, which in turn causes passive coping and stress-related sympathetic overreactivity and higher norepinephrine levels. The authors suggest that these factors contribute to worsening of symptoms. However, although stress responses may exacerbate symptoms it is now generally accepted that there is no common psychological profile of people who have CRPS (Lynch, 1992). Rather, it is believed that CRPS leads to anxiety and depression rather than anxiety and depression leading to CRPS. This is a phenomenon that continues to be the subject of interesting research that has mixed results. For example, Harden et.al. (2003) found that preoperative distress and pain had modest utility in predicting CRPS signs, although there was a high rate of false positive identification. More research is needed to help clarify the relationship between psychological profile, psychogenic predisposition, and CRPS.
Diagnostic tests for CRPS
Diagnostic testing that identifies common parameters of physiologic functioning could be helpful in investigating the possible intersection of CRPS and SMD. However, there is no specific diagnostic test for CRPS. Several medical tests can be used to assist in the diagnosis. Bone scans (Schiepers, 1997) use radiation to identify areas of bone where there may be abnormalities. Infrared thermography (Gulevich, et.al., 1997) measures relative temperature distributions in the limb which may provide information about blood flow and sympathetic activity. Axon reflex testing (Chelimsky, et.al., 1995; Low, Caskey, Tuck, Fealey, & Dyck, 1983), and resting skin temperature/resting sweat output (Chelimsky, et.al., 1995) have also been described in the literature. These are nervous system tests that provide specific information regarding autonomic functioning. Selective tissue conductance (National Pain Foundation, 2003) is a newer diagnostic test that measures galvanic skin responses but it has not been well researched.
In some cases, a sympathetic nerve block can be used to diagnose CRPS in patients with clinical evidence of sympathetically mediated pain; however, not all CRPS is due to sympathetic nerve dysfunction (Rho, Brewer, & Wilson, 2002). Some researchers have tried to identify patients who are at higher risk for CRPS based on other factors including psychological profile, genetics, and sensory processing but none of these are widely accepted and used for diagnostic purposes.
Diagnosis is generally made by the presence of clinical signs and symptoms including dramatic changes in the color and temperature of the skin over the affected limb or body part, intense burning pain, skin sensitivity, sweating, swelling, decreased joint mobility, and changes in nail and hair growth patterns (NINDS, 2003). Additionally, the physician will gather important patient history and rule out any other conditions.
Diagnostic tests for sensory modulation disorders
Pfeiffer & Kinnealey (2003) describe the use of the Adult Sensory Questionnaire (Kinnealey & Oliver, 2002) to determine degree of sensory modulation difficulty but this tool is not widely accessible or commonly used. Kinnealey & Fuiek (1999) also used the Adult Sensory Questionnaire and proposed a model of interrelationship between SMD, anxiety, depression, and pain perception in adults although they noted that more research was needed to clarify these relationships. Preliminary studies (McIntosh, Miller, Shyu, & Hagerman, 1999) support the presence of a physiological basis of SMD, finding that electrodermal responses were larger in children with SMD, excepting those who were non-responders. Additionally, children with atypical electrodermal responses had more parent-reported abnormal behavioral responses to sensation. Miller, et.al. (1999) identified Fragile X syndrome as a clinical condition where baseline hyperarousal may exist because unimodal over-reaction predicted hyperarousal in other sensory modalities. Additionally, Schaaf, Miller, Sewell, & O'Keefe (2003) found that cardiac vagal tone index was significantly decreased for children who had identified sensory processing difficulties. These studies provide preliminary evidence that there is a physiological basis for SMD. All of these studies used the Sensory Challenge Protocol (Miller, et.al., 1999) which is a research tool and is not designed for clinical application. A single case study (Reisman & Gross, 1992) using physiological markers of an adult has also been reported to identify improvements following intervention for SMD.
The Sensory Profile is a standardized assessment used by occupational therapists “to measure a child’s sensory processing abilities and to profile the effect of sensory processing on functional performance in the daily life of a child” (Dunn, 1999, p. 1). Dunn states that there is a relationship between neurological sensory thresholds and observed behavior (1997). The Sensory Profile (Dunn, 1999) provides an assessment of this relationship based on the report of the child’s parent. The Adolescent/Adult Sensory Profile (Brown & Dunn, 2002) provides an assessment of this relationship based on self-report. These measures are the most widely used and widely accepted standards used by occupational therapists for assessing SMD.
Summary of diagnostic tests
Both CRPS and SMD are disorders that are not easily identified and are typically diagnosed through the use of tools that involve clinical observations of presenting symptoms or a report of those symptoms. Researchers often measure neurophysiologic characteristics to determine the presence of each disorder. Many of those neurophysiologic markers are common to both disorders in that they represent altered sympathetic/autonomic functioning; however, most of those tests are not easy to administer in a clinical environment.
The Adolescent/Adult Sensory Profile (AASP) represents a behavioral self-report of sensory processing. The AASP measures four quadrants of sensory processing as identified by Brown and Dunn (2002). The four quadrants include sensation seeking, sensation avoiding, sensory sensitivity and low registration. Preliminary studies suggest that this format of assessment is an accurate predictor of altered neurophysiologic functioning. Specifically, this four quadrant model was validated through expert rating and skin conductance testing (Brown, Tolefson, Cromwell, & Filion, 2001).
The AASP is easy to administer and it is non-invasive. As there seem to be common underlying features of CRPS and SMD relating to altered sympathetic functioning, this assessment may be clinically useful for predicting sympathetic hyperarousal that may potentially lead to CRPS. Additionally, if the assessment is sensitive enough to identify the relationship between CRPS and SMD it may provide evidence of a common underlying neurological deficit between the two conditions.
Face validity for the use of the AASP for predicting CRPS
The Adolescent/Adult Sensory Profile is a sixty item self report questionnaire designed as a “trait measure” (Brown & Dunn, 2002, p.1) of sensory processing, meaning that the individual is supposed to answer regarding how they generally respond to sensory stimulation. It does not measure specific response patterns to specific sensory stimulation. The AASP measures responsivity across categories of taste/smell processing, movement processing, visual processing, touch processing, activity level, and auditory processing (p.2). From these scores the assessment provides a profile of sensory processing across four quadrants: low registration, sensation seeking, sensory sensitivity, and sensation avoiding (p.1.). Dunn’s Model of Sensory Processing (1997) is used to explain the relationship between altered neurological thresholds and the impact that this has on daily life functioning.
Based on previously identified evidence of altered sensory thresholds leading to pain and hyperarousal in people who have CRPS, it seems reasonable to apply Dunn’s model to this population. Although the exaggerated state of sympathetic arousal in people who have CRPS is not clinically identical to hyperarousal in people who have SMD, these two conditions may constitute a continuum of pathology that is reflective of sympathetic nervous system dysfunction.
Literature review does not provide information regarding any possible connections between these disorders, although the presence of parallel studies that examine neurophysiologic/sympathetic markers is intriguing. Occupational therapists who understand these two conditions may assist in elucidating common features that will assist in understanding both CRPS and SMD. The significance of this inquiry is considerable. The ability to identify the population of people who are ‘at-risk’ for developing CRPS would be invaluable for clinical purposes of intervention planning. The significance of this is even greater if this can be determined through the use of a non-invasive self-report questionnaire like the AASP. Additionally, there is only beginning physiologic rationale and understanding of SMD. If a link is present between these disorders CRPS may provide an interesting presentation of sensory-affective hyperarousal that can help occupational therapists better understand SMD and how it impacts occupation.
Summary
Complex regional pain syndrome and sensory modulation disorder are clinically distinct entities that are often treated by different populations of occupational therapists. As a result, there has not been any literature describing or exploring any intersection of these disorders. There has not been any documentation of discussion regarding the intervention strategies that overlap and address similar underlying components of both disorders.
Both disorders are poorly understood, but hyperarousal and excessive sympathetic nervous system outflow are suspected as being significant contributors to both of these disorders. Sympathetic stress loading techniques are commonly used as intervention for both conditions.
Occupational therapy researchers are conducting studies regarding neurophysiologic parameters that would help to quantify sympathetic nervous system hyperarousal. Similar testing techniques have already been used in researching complex regional pain disorders.
Because of multiple points of commonality, assessment strategies useful for sensory modulation disorders may provide useful clinical information regarding complex regional pain syndrome. In turn, these points of commonality could provide a stronger basis of neurophysiologic rationale behind the explanation of sensory modulation disorders.
This paper describes an initial attempt at investigating the intersection of these two disorders. Researching the similarities between these two conditions provides useful clinical information that can lead to better understanding of the disorders and improved intervention strategies and patient outcomes.
II. Methodology
Sample size and composition:
Five subjects were identified for participation in the study. The subjects were all over eighteen years of age. Subject criteria stated that they could be either male or female, but had to be English speaking and residents of the Counties of Erie or Niagara in New York State. All subjects had to have a current diagnosis or recent history of complex regional pain syndrome secondary to orthopedic injuries including fractures, ligament or tendon injuries, or peripheral nerve damage.
The principal investigator provided eligibility criteria to the lead therapist at the ABC Therapeutics facility in Lockport, NY. Based on the criteria, the lead therapist used purposive sampling to develop a subject eligibility list. Subjects were then given an invitation to participate in the study. After subjects expressed interest to participate in the study, all personal and confidential information was de-identified and presented to the principal investigator. Patient charts were never viewed by the principal investigator.
Purposive sampling was used with specific selection criteria as follows: all subjects had to have current or historical clinical signs of complex regional pain syndrome; they had to be over 18 years of age at the time of their initial injury, and they were drawn from the patient pool at a private occupational therapy practice in Lockport, New York. None of the subjects will be patients of the principal investigator. Maximum variation sampling was used regarding subject gender, underlying orthopedic condition, educational attainment, and job title.
Informed consent:
Subjects who expressed an interest in participating were contacted for an appointment to discuss the study with the principal investigator and to sign the informed consent paperwork. During this appointment the principal investigator provided informed consent information to the subject to read. The principal investigator answered all questions relating to the study and the informed consent forms and followed the format as listed on the signature sheets. Once the informed consent process was completed, the subjects were invited to stay to complete the two assessments. Additional appointment times to accommodate the subject’s schedules were provided, as necessary.
Methods and Procedures
Following selection and informed consent processes, the principal investigator provided subjects with the Adolescent/Adult Sensory Profile (AASP) (Brown & Dunn, 2002) to complete. The AASP is a standardized assessment used by occupational therapists to measure sensory processing abilities and to profile the effect of sensory processing on functional performance in daily life. Dunn states that there is a relationship between neurological sensory thresholds and observed behavior (1997). The AASP (Brown & Dunn, 2002) provides an assessment of this relationship based on self-report. This measure is the most widely used and widely accepted standard used by occupational therapists for assessing SMD in adults.
Following completion of the AASP, the principal investigator administered the Canadian Occupational Performance Measure (COPM) to the subject. The COPM (Law, et. al., 1990) is an individualized, client-centered measure designed for use by occupational therapists. The COPM measures self-care, productivity and leisure outcomes. Clients rate themselves on performance and satisfaction with performance.
It is primarily designed to be used as a clinical outcome measure and is cited extensively in the occupational therapy literature. The COPM showed good evidence of concurrent criterion validity and sensitivity to change when used to measure performance after client participation in a pain management program (Carpenter, Baker, & Tyldesley, 2001).
The authors of the COPM identify that it can also be used as a measure of occupational performance in research (Law, et. al., 1990). Specifically, the authors suggest that the COPM is useful for studies aimed at understanding the determinants of occupational performance problems as well as for explanatory studies that try to show relationship between occupation and other variables. For purposes of this study, the COPM was administered once to obtain data on the subject’s perception regarding occupational performance difficulties. It was chosen for this study specifically because it elicited information regarding quality of life and satisfaction with current occupational participation (Liddle & McKenna, 2000).
Although purposive and maximum variation sampling strategies were used, the subject pool had some common characteristics. In summary, they were all within the range of 45-65 years of age. All of the subjects had a diagnosis of complex regional pain syndrome secondary to an injury. Their job titles were significantly variable and although three of the five subjects had distal upper extremity fractures, not all of them were caused by work injuries. Only one subject had education beyond high school. Three women and two men agreed to participate in the study.
The following table outlines demographic characteristics of the subject pool.
Using descriptive methods, information obtained from the AASP was graphically tabulated and analyzed to report frequencies and distributions of scores. Information from the COPM was analyzed with identical methods to report frequencies and distributions of self-reported occupational performance difficulties. Information from the COPM provided additional narrative information that assisted in descriptive analysis.
III. Results
The subjects were given the Adolescent/Adult Sensory Profile to complete. The AASP classifies responses into categories of Low Registration, Sensation Seeking, Sensory Sensitivity, and Sensation Avoiding. Scores are classified as being much less than most people, less than most people, similar to most people, more than most people, and much more than most people.
Low registration refers to a pattern of sensory processing that is characterized by high sensory thresholds and a passive self regulation strategy (Dunn, 1997). Three of the five subjects scored differently than the normative group. Two had a greater degree of low registration and one had a lower degree of low registration.
Sensation seeking refers to a pattern of sensory processing that is characterized by high sensory thresholds and an active self regulation strategy (Dunn, 1997). Two of the five subjects had lower sensation seeking scores than the normative group.
Sensory sensitivity refers to a pattern of sensory processing that is characterized by low sensory thresholds and a passive self regulation strategy (Dunn, 1997). Two of the five subjects scored differently than the normative group: one had a greater degree of sensory sensitivity and one had a lower degree.
Sensation Avoiding refers to a pattern of sensory processing that is characterized by low sensory thresholds and an active self regulation strategy (Dunn, 1997). One subject scored lower than the normative group and one scored much lower than the normative group. Another subject scored much higher than the normative group.
The following table summarizes score performance of the subject pool.

Finally, the subjects were given the Canadian Occupational Performance Measure to complete. Using the COPM scoring card the client was asked to rate the importance of each chosen activity on a scale of 1-10, (1 as not important at all and 10 as extremely important). After reviewing the ratings with the client, the top five highest scored, self- perceived problems were scored for performance and satisfaction. These were also rated on a scale of 1-10. Each score was then divided by 5 (the number of problems identified by the client).
The following table summarizes reported scores of the subject pool.

As indicated in the chart below, the most common problems highlighted by the subjects were inability to complete various aspects of dressing occupations (8 prioritized problems) and inability to work at all (5 prioritized problems). In the leisure category, two subjects specifically identified inability to participate in grandparenting occupations as a prioritized problem. The remaining prioritized problems scattered around individual tasks within the three occupational domains.

IV. Discussion
In this small sample there was evidence that all of the subjects had areas of atypical sensory processing as measured by the AASP. However, there was absolutely no consistency whatsoever in the pattern and distribution of scores on this test. The AASP measures sensory processing differences in a bidirectional manner – meaning that scores can either be higher or lower than the normative range and are considered atypical in either direction away from the mean. However, the nature of that atypicality is dependent on the directionality of difference of the scores.
As identified in the literature review there is some evidence of altered sensory thresholds leading to pain and hyperarousal in people who have CRPS. However, there was not a significant pattern of sensory sensitivity that was seen in the AASP test scores of the subjects. There are several factors that could explain why this relationship was not observed.
First, there may in fact be no relationship to CRPS hyperarousal and pre-existing sensory sensitivity as measured by the AASP. The literature provides strong face validity to the hypothesis that sensory sensitivity and the associated active sensory avoiding behaviors might be associated with the sensory processing of people who have CRPS. However, the patients in this study may have been at different stages with their CRPS and in part that could account for differences in their AASP responses. Very acute CRPS could potentially bias sensory sensitivity responses, where chronic CRPS may not.
Additionally, although the tactile hypersensitivity factors account for a degree of overall hypersensitivity scores, there are other sensory channels that are considered on the AASP. So simple tactile hypersensitivity is only a component of overall sensory sensitivity and may not be enough to trigger identification as in the sensory sensitivity quadrant on the AASP.
Second, the sample size may be too small to identify a reliable measure of sensory processing tendencies of the group. So although it is interesting that the scores of the subjects all were atypical, it is not possible to draw conclusions on this finding at this time.
It may be possible that people who have CRPS are more likely to have sensory processing disturbances that manifest atypically in directions of both hyper and hypo-arousal and responsivity. The AASP measures both behavioral responses and actual sensory perceptions. Depending on an individual’s passive or active coping strategy the nature of the difficulty may be more complex than a simple univariate model that is explained by sensitivity associated with heightened avoidance strategies. Additional research is warranted to elucidate the scoring patterns observed in this initial probe.
More directly, the subject’s prioritization and ranking of perceived occupational performance problems was clear. The subjects report significant problems with loss of ability to participate in preferred occupations, with self care being the greatest area of concern. Work and leisure concerns were also reported, but not at the same frequency. Not all disability or disease processes have a direct relationship to decreases in functional performance. In this case, whether or not there is any underlying relationship between sensory processing factors between CRPS and SMD, it is very clear that people who have these diagnoses experience significant occupational dysfunction. Self care skills and performance in daily activities are domains of concern for occupational therapists. The low COPM scores in perceived performance and satisfaction validates that people who have CRPS with SMD are good candidates for occupational therapy evaluation and intervention.
V. Summary
Complex regional pain syndrome and sensory modulation disorder are clinically distinct entities that are often treated by different populations of occupational therapists. As a result, there has not been any literature describing or exploring any intersection of these disorders. There has not been any documentation of discussion regarding the intervention strategies that overlap and address similar underlying components of both disorders.
Both disorders are poorly understood, but the literature indicates that hyperarousal and excessive sympathetic nervous system outflow are suspected as being significant contributors to both conditions. Sympathetic stress loading techniques are commonly used as intervention for both conditions. Occupational therapy researchers are conducting studies regarding neurophysiologic parameters that would help to quantify sympathetic nervous system hyperarousal. Similar testing techniques have already been used in researching complex regional pain disorders.
Because of these multiple points of commonality between the conditions, assessment strategies useful for sensory modulation disorders were used in this study to obtain additional clinical information regarding complex regional pain syndrome. Although there was no single pattern of sensory processing disorder for people who had CRPS, it was clear that they all had some degree of atypical sensory processing as measured by the AASP. Additionally, all of the subjects who had CRPS had significant occupational dysfunction as measured on the COPM.
VI. Conclusion
The research that has been completed on CRPS provides useful information for occupational therapists to consider when investigating sensory modulation disorders. This literature review and exploratory study demonstrates that there is justification for continuing to study the possible relationship between disorders that share common sensory processing factors as they have a significant impact on people’s occupational function.
References:
Apkarian, A.V., Thomas, S., Krauss, B.R. and Szeverenyi, N.M. (2001). Prefrontal hyperactivity in sympathetically mediated chronic pain. Neuroscience Letters, 311, 193-197.
Ayres, A.J. (1979). Sensory integration and the child. Los Angeles: WPS.
Baron, R. & Wasner, G. (2001). Complex regional pain syndromes. Current Pain and Headache Reports, 5, 114-123.
Brown, C., Tolefson, N., W., Cromwell, R. & Filion, D. (2001). The adult sensory profile: Measuring patterns of sensory processing. American Journal of Occupational Therapy, 55, 75-82.
Brown, C.E. & Dunn, W. (2002). Adolescent/Adult Sensory Profile User’s Manual. San Antonio: The Psychological Corporation.
Carlson. L & Watson, H. K. (1988). Treatment of reflex sympathetic dystrophy using the stress loading program. Journal of Hand Therapy, 1, 149-154.
Carpenter, L. Baker, G.A. & Tyldesley, B. (2001). The use of the Canadian Occupational Performance Measure as an outcome of a pain management program. Canadian Journal of Occupational Therapy , 68(1), 16-22.
Chelimsky, T.C., Low, P.A., Naessens, J.M., Wilson, P.R., Amadio, P.C., O'Brien, P.C, (1995). Value of autonomic testing in reflex sympathetic dystrophy. Mayo Clinic Proceedings, 70, 1029-1040.
Drummond P.D., Finch, P.K., Skipworth, S., & Blockey, P. (2001). Pain increases during sympathetic arousal in patients with complex regional pain syndrome. Neurology 5, 1296-1303.
Dunn, W. (1997). The impact of sensory processing abilities on the daily lives of young children and their families: A conceptual model. Infants and Young Children, 9, 23-35.
Dunn, W. (1999). Sensory Profile User’s Manual. San Antonio: The Psychological Corporation.
Gulevich, S.J., Conwell, T.D., Lane, J., Lockwood, B., Schwettmann, R.S., Rosenberg, N., et.al. (1997). Stress infrared telethermography is useful in the diagnosis of complex regional pain syndrome, type I (formerly reflex sympathetic dystrophy), Clinical Journal of Pain, 13, 50-59.
Harden, R.N., Bruehl, S., Stanos, S., Brander, V., Chung, O.Y., Saltz, S. et.al. (2003). Prospective examination of pain-related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: A preliminary study. Pain, 106, 393-400.
Janig, W. & Baron, R (2002). Complex regional pain syndrome is a disease of the central nervous system. Clinical Autonomic Research, 12, 150-164.
Janig, W. & Baron, R (2003). Complex regional pain syndrome: mystery explained?
The Lancet Neurology, 2, 687-97.
Juottonen, K., Gockel, M., Silen, T., Hurri, H., Hari, R., & Forss, N. (2002). Altered central sensorimotor processing in patients with complex regional pain syndrome. Pain. 98, 315-23.
Kandel, E.R. & Jessell, T.M.(2001). Touch, in Kandel, E.R., Schwartz, J.H. & Jessell, T.M. (Eds.). Principles of Neural Science, 3rd ed. New York: Elsevier.
Kinnealey M.., Fuiek, M. (1999) The relationship between sensory defensiveness, anxiety, depression and perception of pain in adults. Occupational Therapy International. 6, 195-206.
Kinnealey, M. & Oliver, B. (2002). The Adult Sensory Questionnaire. Retrieved July 17, 2004 from http://www.temple.edu/OT/Neuro_Behavioral_Center2.htm
Law, M., Cooper, B., Strong, S., Stewart, D., Rigby, P., & Letts, L. (1996). The Person-Environment-Occupation Model: A transactive approach to occupational performance. Canadian Journal of Occupational Therapy, 63, 9-23.
Law, M., Baptiste, S., McColl, M.A., Opzoomer, A., Polatajko, H. & Pollock, N. (1990). The Canadian Occupational Performance Measure: An outcome measure for occupational therapy. Canadian Journal of Occupational Therapy, 57(2), 82-87.
Liddle, J & McKenna, K. (2000). Quality of Life: An overview of issues for use in occupational therapy outcome measurement. Australian Occupational Therapy Journal, 47, 77-85.
Low, P.A., Caskey, P.E., Tuck, R.R., Fealey, R.D., Dyck, P.J. (1983). Quantitative sudomotor axon reflex test in normal and neuropathic subjects. Annals of Neurology, 14, 573-580.
Lynch, M. (1992). Psychological aspects of reflex sympathetic dystrophy: a review of the adult and paediatric literature. Pain. 49, 337-347.
Maihofner C., Handwerker, H.O., Neundorfer, B., Birklein, F. (2003). Patterns of cortical reorganization in complex regional pain syndrome. Neurology, 61, 1707-15.
Maleki, J., LeBel, A.A., Bennett, G.J., & Schwartzman, R.J. (2000). Patterns of spread in complex regional pain syndrome, type I (reflex sympathetic dystrophy). Pain, 88, 259-66
McIntosh DN, Miller LJ, Shyu V, Hagerman RJ. (1999). Sensory-modulation disruption, electrodermal responses, and functional behaviors. Developmental Medicine and Child Neurology, 41, 608-15.
Melzack, R. & Wall, P. (1965). Pain mechanisms: A new theory, Science, 150, 171-179.
Miller L.J., McIntosh, D.N., McGrath, J., Shyu, V., Lampe, M., Taylor, A.K., et.al. (1999). Electrodermal responses to sensory stimuli in individuals with fragile X syndrome: A preliminary report. American Journal of Medical Genetics, 83, 268-79.
Miller, L. J., Reisman, J. E., McIntosh, D. N., & Simon, J. (2001). An ecological model of sensory modulation: Performance of children with fragile X syndrome, autistic disorder, attention-deficit/hyperactivity disorder, and sensory modulation dysfunction. In S. Smith-Roley, E. I. Blanche, & R. C. Schaaf (Eds.), Understanding the nature of sensory integration with diverse populations (pp. 57-88). San Antonio, TX: Therapy Skill Builders.
National Institute for Neurological Disorders and Stroke (2003). Complex Regional Pain Syndrome (also called Reflex Sympathetic Dystrophy Syndrome) Fact Sheet. Retrieved May 14, 2004 from http://www.ninds.nih.gov/health_and_medical/
pubs/rsds_fact_sheet.htm
National Pain Foundation (2003). How CRPS Happens. Retrieved June 3, 2004 from http://www.painconnection.org/cm/CMDisplayAllArticles.asp?ClassId=15&CategoryId=1
Parham, L.D. & Mailloux, Z. (2001). Sensory integration. In J.Case-Smith (Ed.), Occupational therapy for children (4th ed.). St. Louis: Mosby.
Pfeiffer, B. & Kinnealey, M. (2003) Treatment of sensory defensiveness in adults. Occupational Therapy International, 10, 175-184.
Phillips, M.E., Katz, J.A., & Harden, R.N. (2000). The use of nerve blocks in conjunction with occupational therapy for complex regional pain syndrome type I. American Journal of Occupational Therapy. 54, 544-549.
Reisman, J.E., & Gross, A.Y. (1992) Psychophysiological measurement of treatment effects in an adult with sensory defensiveness. Canadian Journal of Occupational Therapy, 59, 5248-5257.
Rho, R.H., Brewer, R.P., Lamer, T.J., Wilson, P.R. (2002). Complex regional pain syndrome. Mayo Clinic Proceedings, 77, 174-180.
Rommel, O., Malin, J., Zenz, M., & Jänig, W. (2001). Quantitative sensory testing, neurophysiological and psychological examination in patients with complex regional pain syndrome and hemisensory deficits. Pain, 93, 279-293.
Schaaf, R.C., Miller, L.J., Sewell, D., & O'Keefe, S. (2003). Children with disturbances in sensory processing: A pilot study examining the role of the parasympathetic nervous system. American Journal of Occupational Therapy, 57, 442-449.
Schiepers, C. (1997). Clinical value of dynamic bone and vascular scintigraphy in diagnosing reflex sympathetic dystrophy of the upper extremity. Hand Clinics, 13, 423-429.
Schwoebel, J., Friedman, R., Duda, N., Coslett, H.B. (2001). Pain and the body schema: evidence for peripheral effects on mental representations of movement. Brain, 124, 2098-104.
Stanton-Hicks, M., Janig, W., Hassenbusch, S., Haddox, J.D., Boas, R., Wilson, P. (1995). Reflex sympathetic dystrophy: Changing the concepts and taxonomy, Pain: 63, 127-133.
Van Houdenhove, B., & Vasquez, G. (1993). Is there a relationship between reflex sympathetic dystrophy and helplessness? General Hospital Psychiatry, 15, 325-329.
Wasner, G., Schattschneider, J., Binder, A., & Baron, R. (2003). Complex regional pain syndrome--diagnostic, mechanisms, CNS involvement and therapy. Spinal Cord. 41, 61-75.
Wilbarger, J.L. & Wilbarger, P.L. (2002). The Wilbarger approach to treating sensory defensiveness, In Bundy, A.C., Murray, E.A., & Lane, S. (Eds.). Sensory Integration: Theory and Practice, 2nd Ed., Philadelphia, PA.: F.A. Davis.
Acknowledgement
Many thanks to Dr. Carol Reed and Dr. Sandee Dunbar who both provided neverending encouragement, review, and editing for this project.


Comments
I'll take some time to respond in more detail to your interesting post.
One thing I just thought I'd mention is that on the whole, CRPS is reasonably easy to identify - there are clear diagnostic criteria and this makes it quite a discernable clinical entity. However, as you know, having a label and being able to use that to treat someone is a very different story! I'm not sure that at this stage a diagnosis is as helpful as a formulation...
I'm also not entirely certain whether the fMRI evidence demonstrates a cause (ie CNS processing dysfunction causing CRPS), or an effect of dysfunction (ie CNS processing changes associated with disrupted function). And clearly it's unethical to carry out a human experimental trial of this!
At this stage I think the best we can say is that fMRI changes are associated with CRPS and certain characteristics such as neglect, reduced proprioception and the presence of pain.
Psychological features of people who have CRPS are similar to (ie no major distinction between) the presentation of people with other chronic pain problems. Again, it's an association rather than any demonstrable causal relationship.
I'll be back though to respond in more detail - or via blog!
cheers
Bronnie